To Induce Protective Immunity Against A Disease, A Vaccine Must Always Provide:
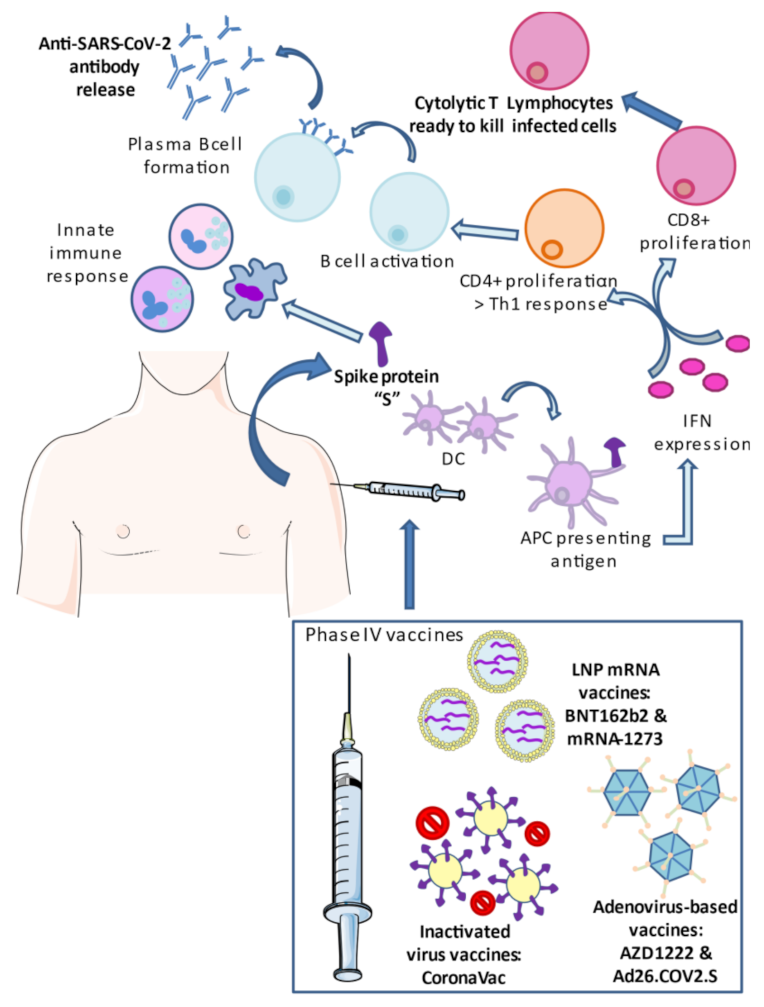
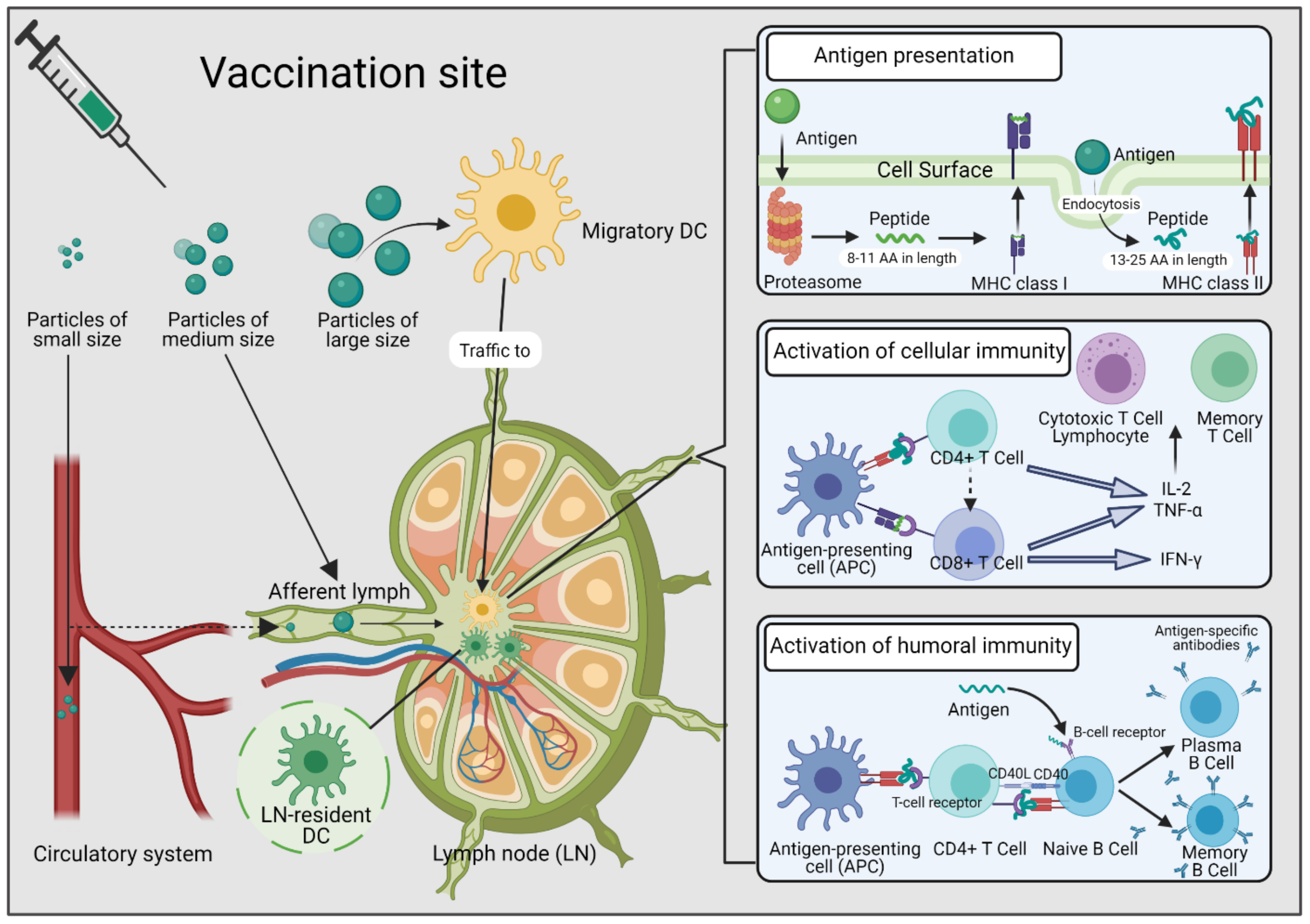
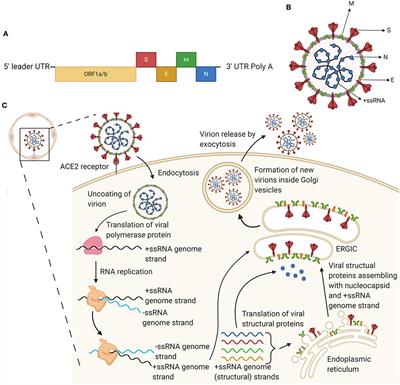
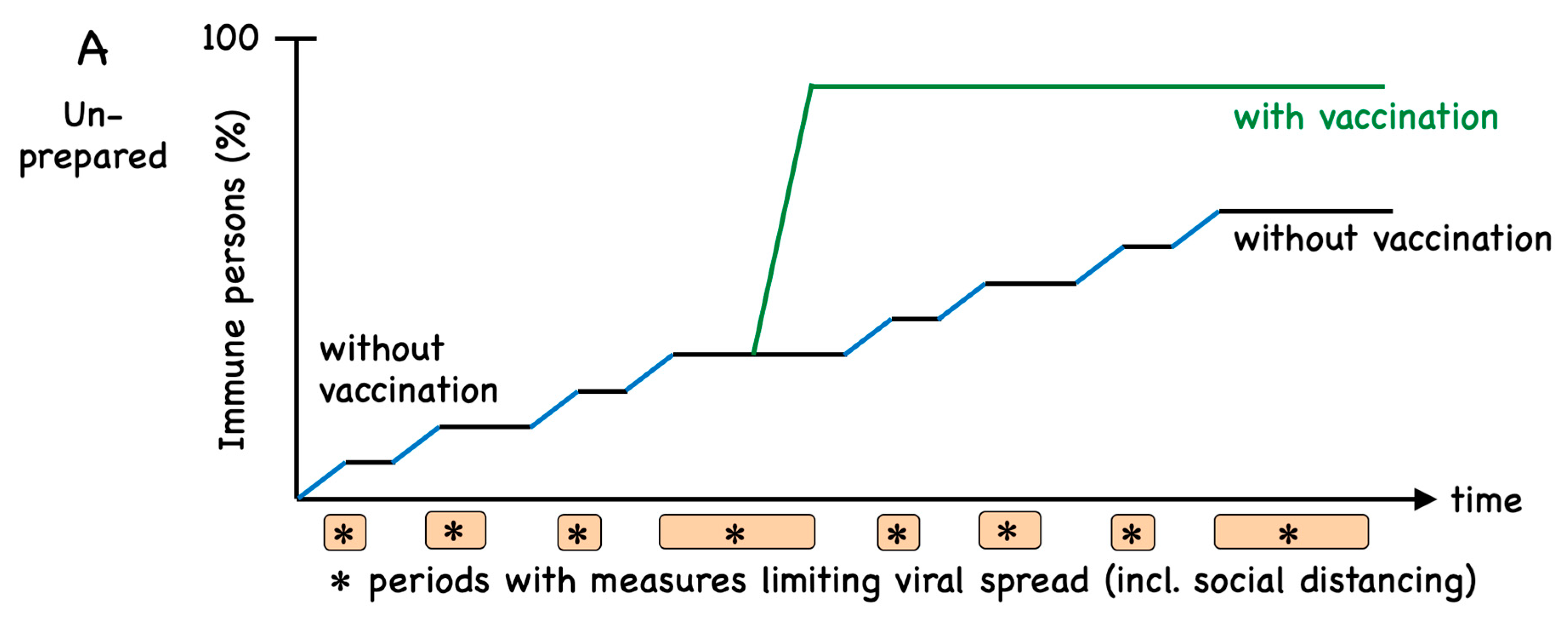
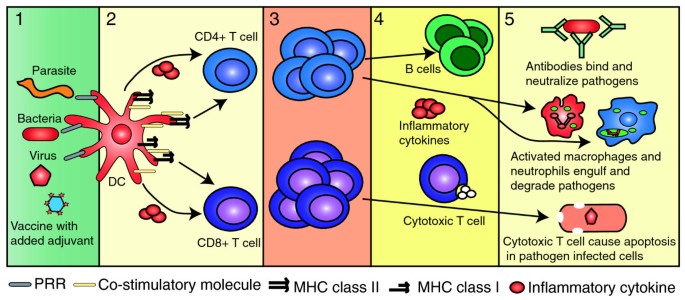
To induce protective immunity against a disease, a vaccine must always provide:. For SARS-CoV-2 researchers are using a multitude of approaches to vaccine development targeting various mechanisms to. When someone is vaccinated they are very likely to be protected against the targeted disease. Antibodies and of immune memory to protection against spe-cic diseases are essential parameters of long-term vaccine efcacy.
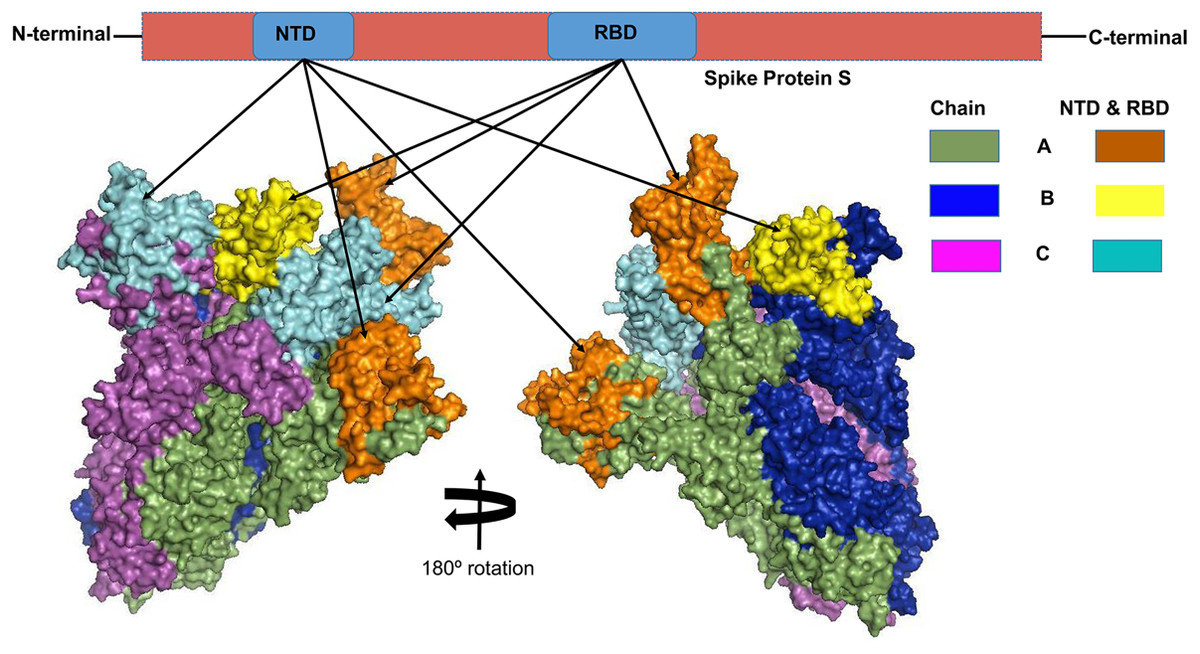
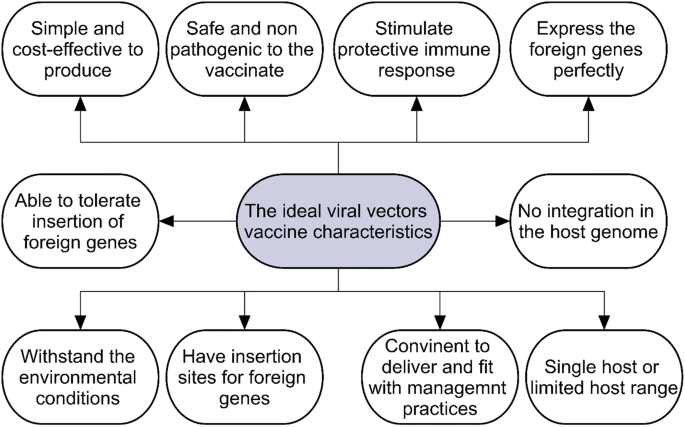
Structural similarity to portions of the microorganism. In reality it is actually extremely difficult to produce vaccines that stop virus infection altogether. Viral-vector vaccines remain the best means to.
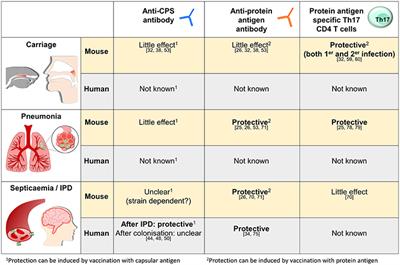
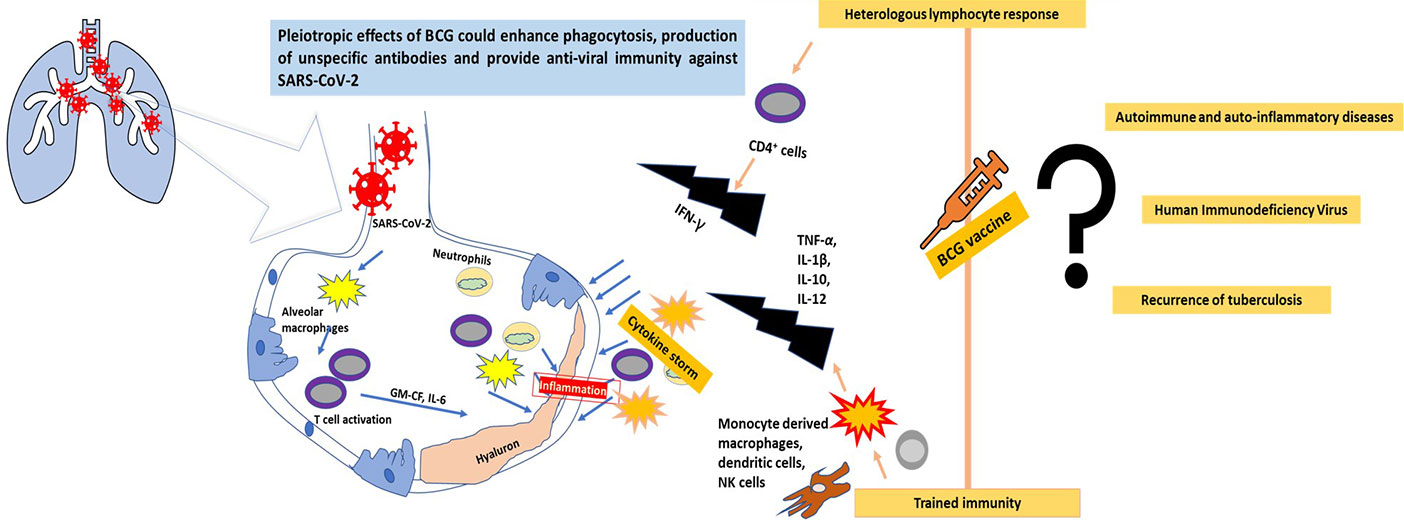
Advances occur as we gain greater insight into the interrelationship of viruses and the immune system. Such vaccine constructs can induce Ag-specific immune responses that protect against mucosal infec. Previous research has demonstrated that influenza-specific T cells can provide broadly heterotypic protective immunity in both mice and humans supporting the rationale for developing a T cell-targeted universal influenza vaccine.
Intact DNA from the microorganism. The progressive loss of protective antibodies against an antigen or disease that occurs with the passage of time. Similarly delivering the coronavirus vaccine directly to the nose may contribute to a stronger mucosal immunity in the nose and lungs offering protection at the.
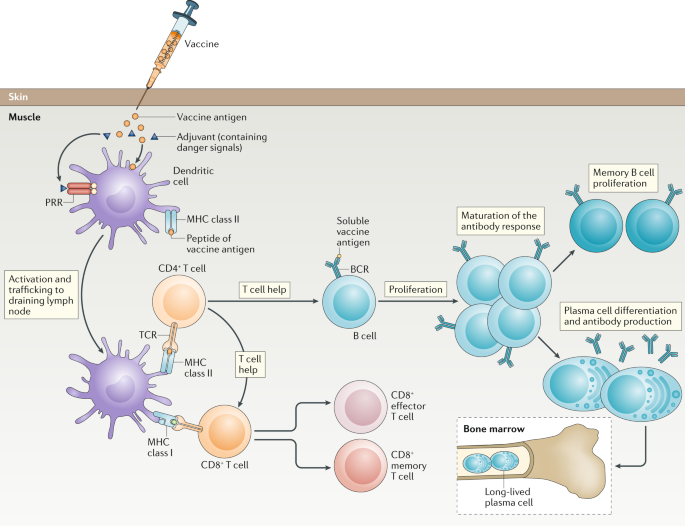
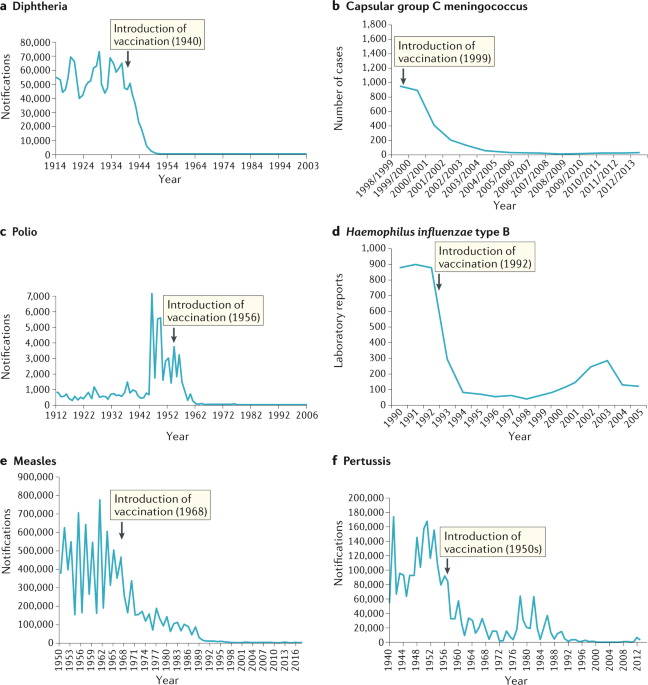
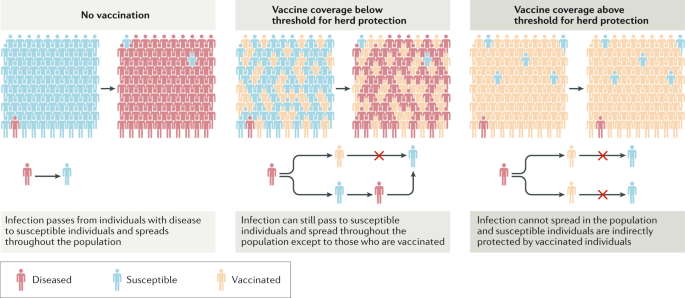
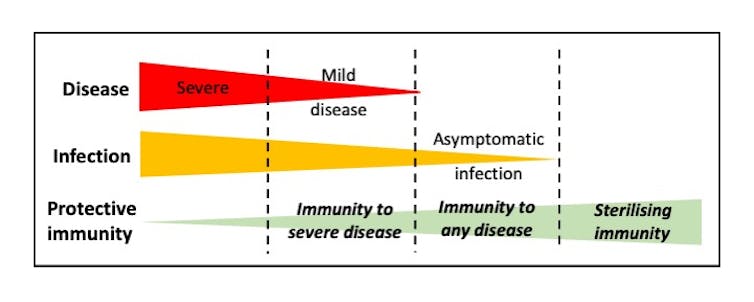
A vaccine typically contains an agent that resembles a disease-causing microorganism and is often made from weakened or killed forms of the microbe its toxins or one of its surface proteins. In an ideal world all vaccines would induce sterilising immunity. New approaches to induce more broadly protective immunity are urgently needed.
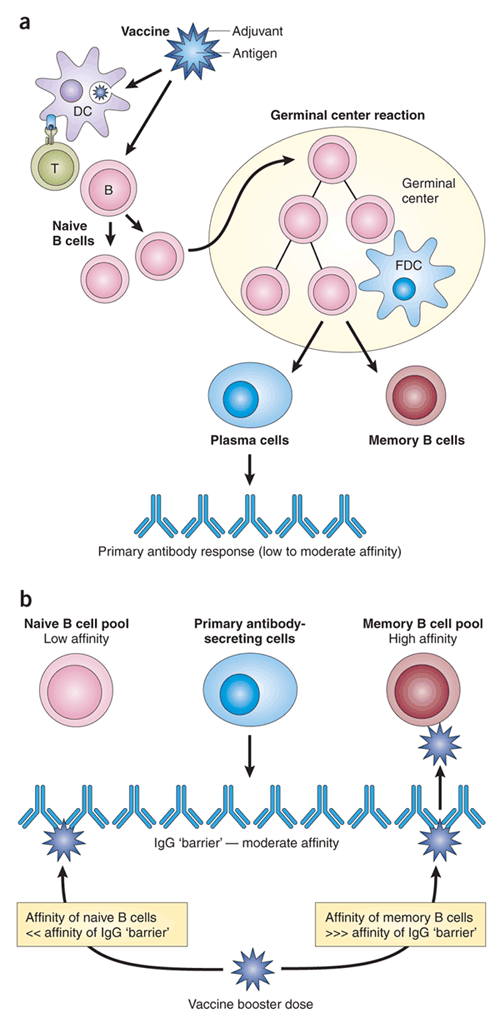
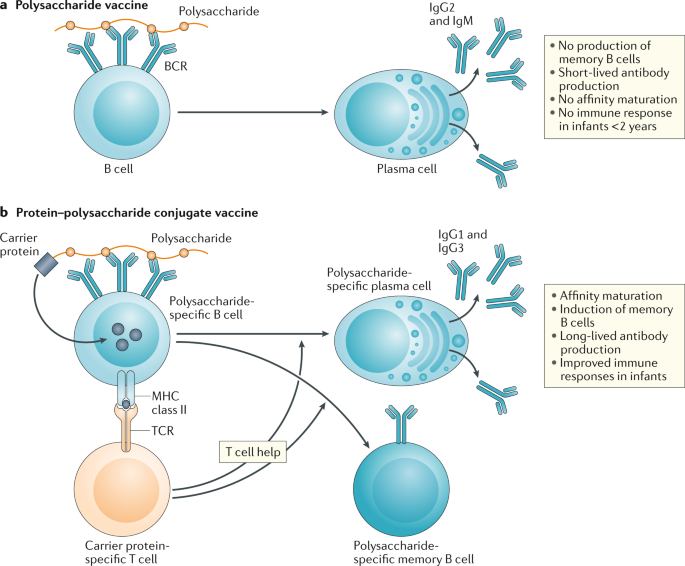
T cells are essential to the induction of high-afnity. Vaccines greatly reduce the risk of infection by working with the bodys natural defenses to safely develop immunity to disease. But a vaccine that provides sterilising immunity stops the virus in its tracks.
But not everyone can be vaccinated. The live disease-causing microorganism.
The main reason for this is that influenza A viruses continue to circulate as antigenic drift variants that have accumulated mutations in antigenic sites of the HA molecule that.
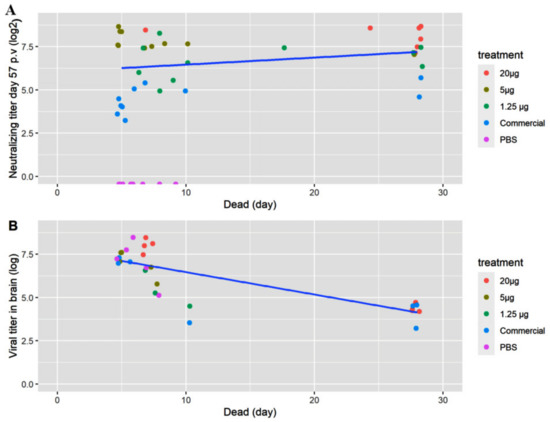
Discussing the findings Professor Eleanor Riley an expert in immunology and infectious disease at the University of Edinburgh said. T cells are essential to the induction of high-afnity. When someone is vaccinated they are very likely to be protected against the targeted disease. Such vaccine constructs can induce Ag-specific immune responses that protect against mucosal infec. Vaccines greatly reduce the risk of infection by working with the bodys natural defenses to safely develop immunity to disease. Haemofelis reinfection and it provides important information for potential future hemoplasma vaccine design. A vaccine typically contains an agent that resembles a disease-causing microorganism and is often made from weakened or killed forms of the microbe its toxins or one of its surface proteins. Most vaccines that are in. It is a crucial factor in vaccination.
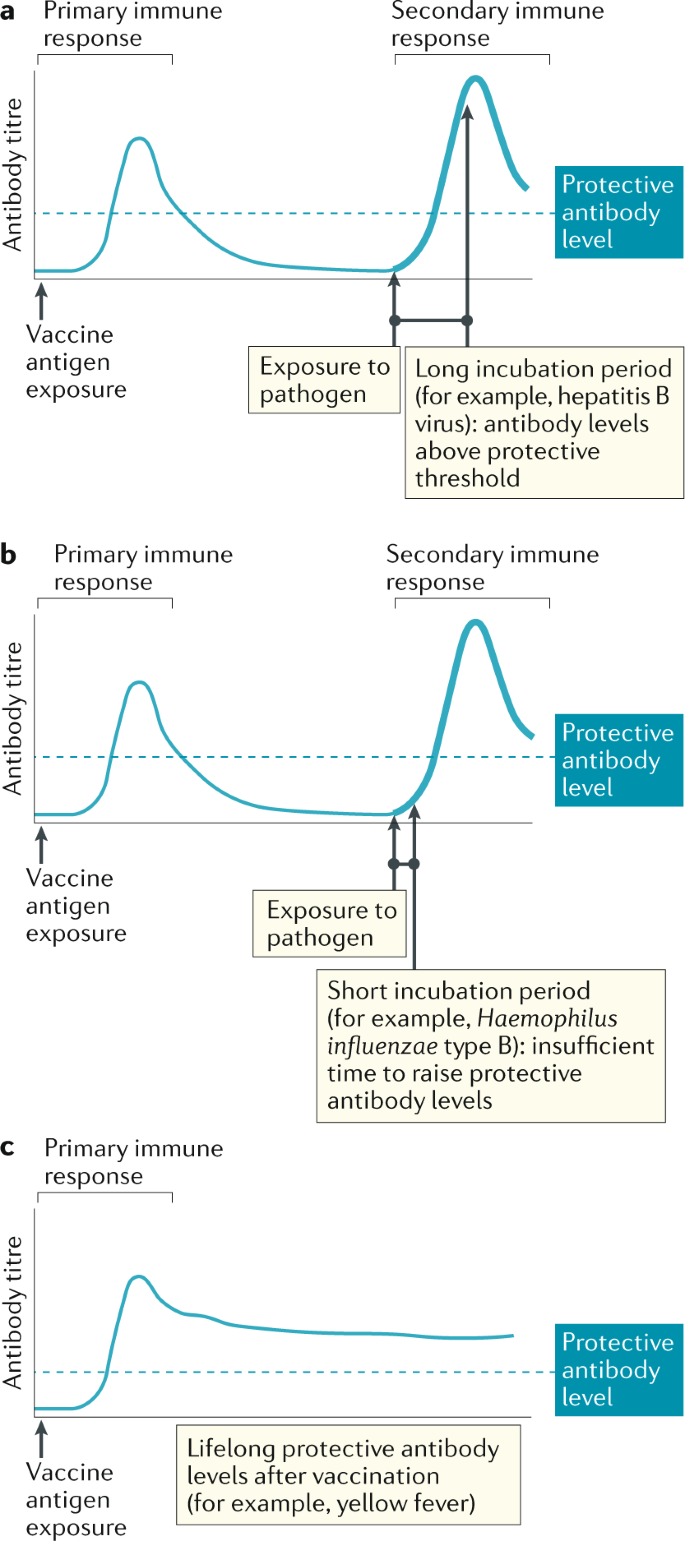
Such vaccine constructs can induce Ag-specific immune responses that protect against mucosal infec. This is the first study to demonstrate protective immunity against M. The predominant role of B cells in the efcacy of current vaccines should not overshadow the importance of T-cell responses. T cells are essential to the induction of high-afnity. Booster doses of a vaccine are given when the immune response to an antigen drops below protective levels. Structural similarity to portions of the microorganism. INTRODUCTION The hemotropic mycoplasmas hemoplasmas are a group of mycoplasmal pathogens that adhere to the surface of red blood cells RBCs and are capable of inducing severe anemia 1.



























Post a Comment for "To Induce Protective Immunity Against A Disease, A Vaccine Must Always Provide:"